Meet Professor ChungAssociate Professor Chung is a urological surgeon specialising in andrology, microsurgical, and urological prosthetic surgery. Contact(07) 3832 1168 |
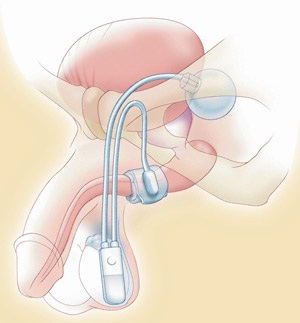
Artificial urinary sphincterThe artificial urinary sphincter is the only device that closely simulates the function of a human biological urinary sphincter and is the treatment of choice in patients with moderate to severe stress urinary incontinence (wears more than 3 pads, describes continuous urine dribble and urinary incontinence at night) as well as in men who have received radiation therapy. This device has been around since the early 1970s and consists of 3-parts; an inflatable cuff that surrounds the urethra, a pressure-regulating balloon (filled with saline) that acts as a fluid reservoir, and a control pump (placed in the scrotum). Manual compression of the pump would cause the cuff to deflate and you can then void. However within a short time frame (usually 30 seconds to 1 minute) the cuff will reinflate due to the transfer of fluid from the pressure-regulating balloon to the cuff and you become dry again. Sometimes you may need to recycle the device a few times to completely empty your bladder. Over the last 40 years, this device has proved to be effective, safe and durable. It is associated with excellent patient satisfaction and restoration of quality of life. Prof. Chung is the leading author of the AMS 800 artificial urinary sphincter guideline - Chung E, Liao L, Kim JH, Wang Z, Kitta T, Lin ATL et al. The Asia-Pacific AMS800 artificial urinary sphincter consensus statement. Int J Urol. 2023;30(2):128-138
What preparation is required?Since an artificial urinary sphincter implant is performed under general anaesthesia, you should have nothing to eat or drink for 6 hours prior to treatment. Regular medications can be taken with a sip of water with the exception of blood thinning agents (eg. warfarin, aspirin, clopidogrel) or non-steroidal anti-inflammatories which need to be stopped for 7-10 days. A midstream urine (MSU) test is required to ensure the urine is sterile before treatment is undertaken. What do I need to bring to surgery?
What happens in the operating room?You will meet your anaesthetist before surgery, who will take a thorough medical history. Your procedure will be performed under general anaesthesia with an anti-microbial cover. The genital area will be shaved and an alcoholic antiseptic will be applied to minimise microbial skin colonisation. What are the risks?Since an artificial urinary sphincter implant involves the insertion of a foreign device, strict microbial prophylaxis and surgical techniques are paramount. When performed by an expert surgeon, an artificial sphincter implant is a safe procedure. Specific complications involve:
Potential serious complications include:
What to expect afterwards?You are usually required to stay overnight to receive intravenous antibiotics for 24 hours postoperatively. Your urinary catheter and surgical dressing will be removed the next morning after your surgery. You will remain incontinent of urine for a time until the artificial sphincter can be safely activated. When you are comfortable and passing urine satisfactory, you will be discharged with 10-14 days of oral antibiotics. At home, you should rest and avoid strenuous physical exertion for 4-6 weeks. Follow-upYou will be contacted or have an appointment the following week in order to check on your progress. The recycling of the artificial urinary sphincter occurs at your second follow-up with Prof. Chung at 4 to 6 weeks postoperatively. During that visit, you should take simple oral analgesia prior to the appointment as you might experience local pain when the artificial urinary sphincter is activated for the first time.
Meet Professor ChungAssociate Professor Chung is a urological surgeon specialising in andrology, microsurgical, and urological prosthetic surgery. Contact(07) 3832 1168 |